100763
论文已发表
提 交 论 文
注册即可获取Ebpay生命的最新动态
注 册
IF 收录期刊
- 3.3 Breast Cancer (Dove Med Press)
- 3.4 Clin Epidemiol
- 2.5 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.5 Clin Interv Aging
- 4.7 Drug Des Dev Ther
- 2.7 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.5 Int J Women's Health
- 2.5 Neuropsych Dis Treat
- 2.7 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.3 Ther Clin Risk Manag
- 2.5 J Pain Res
- 2.8 Diabet Metab Synd Ob
- 2.8 Psychol Res Behav Ma
- 3.0 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.7 Risk Manag Healthc Policy
- 4.2 J Inflamm Res
- 2.1 Int J Gen Med
- 4.2 J Hepatocell Carcinoma
- 3.7 J Asthma Allergy
- 1.9 Clin Cosmet Investig Dermatol
- 2.7 J Multidiscip Healthc

发现对人感染含有 R294K 变异的 H7N9 病毒的潜在药物
Authors He JY, Li C, Wu G
Published Date December 2014 Volume 2014:8 Pages 2377—2390
DOI http://dx.doi.org/10.2147/DDDT.S74061
Received 10 September 2014, Accepted 23 October 2014, Published 1 December 2014
Background: After the first epidemic wave from February
through May 2013, the influenza A (H7N9) virus emerged and has followed a
second epidemic wave since June 2013. As of June 27, 2014, the outbreak of H7N9
had caused 450 confirmed cases of human infection, with 165 deaths included.
The case-fatality rate of all confirmed cases is about 36%, making the H7N9
virus a significant threat to people’s health. At present, neuraminidase inhibitors
are the only licensed antiviral medications available to treat H7N9 infections
in humans. Oseltamivir is the most commonly used inhibitor, and it is also a
front-line drug for the threatening H7N9. Unfortunately, it has been reported
that patients treated with oseltamivir can induce R294K (Arg294Lys)
substitution in the H7N9 virus, which is a rare mutation and can reduce the
antiviral efficacy of inhibitors. Even worse, deaths caused by such mutation
after oseltamivir treatment have already been reported, indicating that the
need to find substitutive neuraminidase inhibitors for currently available
drugs to treat drug-resistant H7N9 is really pressing.
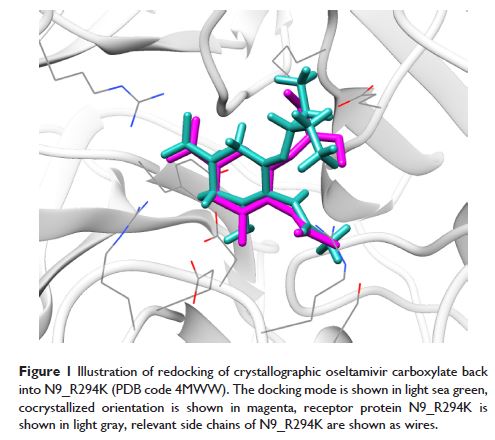
Materials and methods: First,
the structure of H7N9 containing the R294K substitution was downloaded from the
Protein Data Bank, and structural information of approved drugs was downloaded
from the ZINC (ZINC Is Not Commercial) database. Taking oseltamivir carboxylate
as a reference drug, we then filtered these molecules through virtual screening
to find out potential inhibitors targeting the mutated H7N9 virus. For further
evaluation, we carried out a 14 ns molecular dynamic simulation for each
H7N9–drug complex and calculated the binding energy for each candidate drug.
Results: We found five
inhibitors that could be candidate drugs for treating the mutated H7N9 virus.
Docking poses showed these drugs could bind to the virus effectively, with the
contribution of hydrogen bonds and hydrophobic interactions. With regard to the
molecular dynamic simulations, receptor–ligand complexes formed by these
candidate drugs were more stable than the one formed by oseltamivir
carboxylate. The binding energy of oseltamivir carboxylate was -122.4
kJ/mol, while those for these potential inhibitors
were -417.5, -404.7, -372.2, -304.3, and -289.9 kJ/mol, much better
than the reference drug.
Conclusion: Given the current
and future threat of the mutated H7N9 virus, it is urgent that potent drugs and
effective antiviral therapeutics be found. Our study therefore is able to complement
currently available drugs for influenza A infectors and helps to prevent the
ongoing threat of H7N9 virus.
Keywords: H7N9, neuraminidase,
mutation, virtual screening, inhibitor