100763
论文已发表
提 交 论 文
注册即可获取Ebpay生命的最新动态
注 册
IF 收录期刊
- 3.3 Breast Cancer (Dove Med Press)
- 3.4 Clin Epidemiol
- 2.5 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.5 Clin Interv Aging
- 4.7 Drug Des Dev Ther
- 2.7 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.5 Int J Women's Health
- 2.5 Neuropsych Dis Treat
- 2.7 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.3 Ther Clin Risk Manag
- 2.5 J Pain Res
- 2.8 Diabet Metab Synd Ob
- 2.8 Psychol Res Behav Ma
- 3.0 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.7 Risk Manag Healthc Policy
- 4.2 J Inflamm Res
- 2.1 Int J Gen Med
- 4.2 J Hepatocell Carcinoma
- 3.7 J Asthma Allergy
- 1.9 Clin Cosmet Investig Dermatol
- 2.7 J Multidiscip Healthc

已发表论文
顺利获得比较女性卵巢低级别位浆液性癌与那些高级别组织学癌进行的一项生存分析
Authors Chen M, Jin Y, Bi YL, Yin J, Wang YX, Pan LY
Published Date October 2014 Volume 2014:7 Pages 1891—1899
DOI http://dx.doi.org/10.2147/OTT.S67812
Received 15 May 2014, Accepted 8 July 2014, Published 16 October 2014
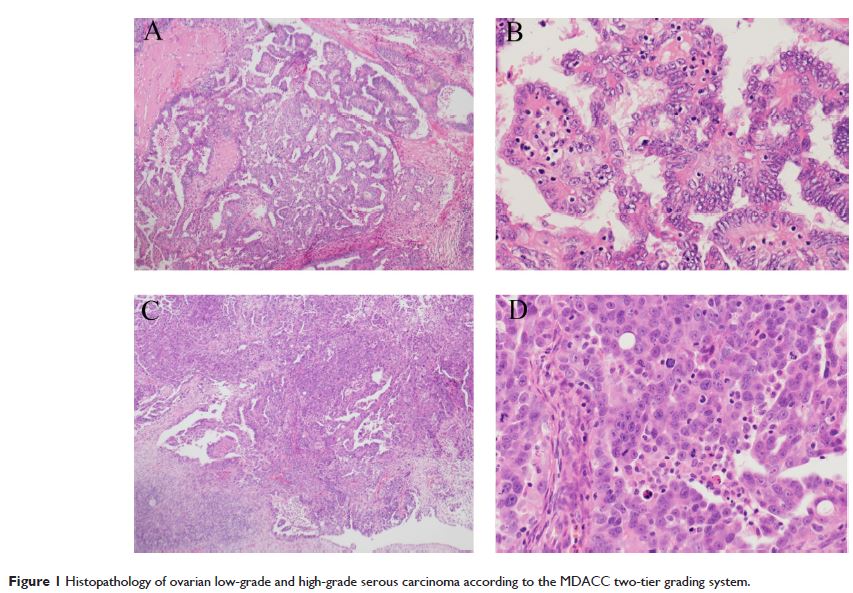
Abstract: Ovarian low-grade serous carcinoma (LGSC) and high-grade serous carcinoma have distinct molecular profiles, clinical behaviors, and treatment responses. The survival advantage for patients with low-grade carcinoma compared with patients with high-grade histology remains controversial. We retrospectively reviewed the medical charts of 381 patients with ovarian serous carcinoma at Peking Union Medical College Hospital from 2007 to 2010. Patients were classified into two groups according to MD Anderson two-tier system: 35 (9.2%) cases with LGSC and 346 with high-grade serous carcinoma. Patients with low-grade serous ovarian cancer had a significantly younger age at diagnosis (46 versus 56 years, P =0.046), and their median progression-free survival (PFS) and overall survival values were 35.0 and 54.0 months, respectively. A multivariate analysis showed that, for serous ovarian cancer, the histological grade was a significant prognostic factor for PFS but not for overall survival (P =0.022 and P =0.0566, respectively). When stratified by the existence of a residual disease, patients with low-grade disease who underwent cytoreductive surgery without macroscopic residual disease (>1 cm) had a significantly improved median PFS time (36.0 months) compared with that of patients with high-grade carcinoma who received optimal cytoreductive surgery (16.0 months, P =0.017). Conversely, patients with low-grade and high-grade carcinoma who were left with macroscopic residue (>1 cm) experienced a similarly shorter median PFS (10.0 and 13.0 months, respectively, P =0.871). The International Federation of Gynecology and Obstetrics stage and residual disease were significant prognostic factors of low-grade carcinoma, while positive ascites was associated with a worse PFS value. Our data showed that LGSC is a different entity from high-grade carcinoma and that LGSC was associated with improved PFS after optimal cytoreductive surgery but not suboptimal operation.
Keywords: ovarian carcinoma, low-grade serous carcinoma, high-grade serous carcinoma, prognosis
Keywords: ovarian carcinoma, low-grade serous carcinoma, high-grade serous carcinoma, prognosis
Download Article[PDF]